Common Bulimia Medical Complications
Bulimia Nervosa is a serious, life-threatening eating disorder characterized by repeated consumption of large amounts of food followed by compensatory behaviors such as self-induced vomiting intended to undo or compensate for the effects of binge eating. Bulimia takes a considerable toll on the body and mind. Medical complications associated with the disorder are common, as the effects of prolonged bulimia can cause sustained damage to bodily functions and organs.
by: Enchi Dai
Eating disorders are lethal, carrying the highest risk of death among all the mental disorders. Today, we are going to focus on one of the most common eating disorders — Bulimia Nervosa. We are going to examine the reasons why it is deadly by addressing its common medical complications, how & where to get properly evaluated for medical concerns, and some different treatment options.
What is Bulimia Nervosa?
Bulimia Nervosa is an emotional disorder involving distortion of body image and an obsessive desire to lose weight, in which bouts of extreme overeating are followed by self-induced vomiting, purging, or fasting. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the diagnostic criteria for Bulimia Nervosa are:
A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
1. Eating, in a discrete period of time (e.g., within any 2-hour period), an amount of food that would be considered larger than what most individuals would eat in a similar period of time under similar circumstances.
2. A sense of lack of control overeating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating).
B. Recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise.
C. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months.
D. Self-evaluation is unduly influenced by body shape and weight.
E. The disturbance does not occur exclusively during episodes of Anorexia Nervosa.
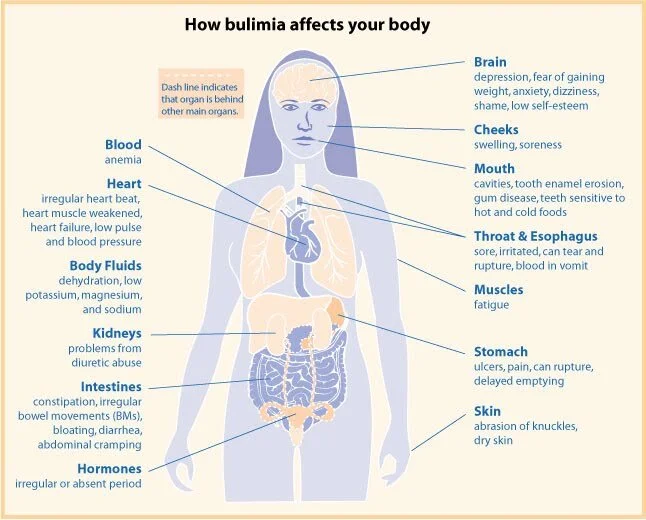
Common Medical Complications of Bulimia Nervosa & Why It Is Fatal
Source: National Women’s Health Information Center
As indicated in the diagram, Bulimia Nervosa affects the whole body.
Common Symptoms:
Behavioral: binge eating, compulsive behavior, impulsivity, self-harm, vomiting after overeating, or lack of restraint
Whole-body: dehydration, fatigue, food aversion, hunger, or water-electrolyte imbalance
Mood: anxiety, general discontent, guilt, or mood swings
Mouth: bad breath, dental cavities, or dryness
Gastrointestinal: constipation, heartburn, or inflamed esophagus
Weight: bodyweight changes or weight loss
Menstrual: the absence of menstruation or irregular menstruation
Others: abnormality of taste, depression, poor self-esteem, or sore throat
How Deadly Is It?
Research has shown that the crude mortality rate for Bulimia Nervosa is 3.9% (Crow et al., 2009). In another study, researchers followed up with 258 individuals with Bulimia Nervosa for an average of 10.5 years. They found that individuals with severe Bulimia Nervosa are at a higher risk of death (mainly suicide) especially with previous suicide attempts or previously low BMI (Huas et al., 2012).
Evaluations for Medical Concerns
We’ve discussed the health risks associate with Bulimia Nervosa, now a medical evaluation is necessary to assess clients for these complications in order to determine whether hospitalization is necessary. Annual health supervision examinations and preparticipation sports physicals both are ideal screening opportunities. A medical evaluation usually includes—
Medical history
Physical examination: weight and height; vital signs including heart rate, blood pressure both supine and standing, and temperature; cardiovascular assessment; and skin examination.
Laboratory assessment: serum electrolytes, blood urea nitrogen, serum creatinine, serum glucose, liver function tests, etc.
Excluding medical disorders: neoplasm, chronic infections, uncontrolled diabetes mellitus, hyperthyroidism, etc.
Treatment Options
Early diagnosis and treatment intervention can make a huge difference in the prognosis (the expected development of an illness) of Bulimia Nervosa. According to Mayo Clinic, evidence has indicated that the following types of psychotherapy may help improve symptoms of Bulimia Nervosa:
Cognitive behavioral therapy (CBT): helps normalize eating patterns, identify unhealthy negative beliefs and behaviors, and replace them with healthy positive one.
Family-based treatment (FBT): helps parents intervene to stop their teenager's unhealthy eating behaviors; it helps the teen regain control over his or her eating; and it also assists the family in dealing with problems that bulimia can have on the teen's development and the family.
Interpersonal psychotherapy (IPT): addresses difficulties in clients’ close relationships, helping to improve their communication and problem-solving skills.
At BALANCE eating disorder treatment center, we treat the spectrum of eating disorders, including anorexia, bulimia, binge eating disorder, compulsive overeating, and other disordered eating behaviors and body image issues. We offer a variety of virtual programs and services to help our clients not only reduce eating disorder symptoms but also move toward a more harmonious relationship with food and their bodies. Click the button below to browse our full selection of virtual programs & services.
This post was written by BALANCE Blog Intern, Enchi Dai.
Enchi is a Bachelor's-Master's student at New York University, majoring in Psychology. After her recovery from disordered eating, Enchi became passionate about spreading ED awareness, advocating for intuitive eating, and promoting Health at Every Size. Enchi is also an ACE Certified Personal Trainer and Registered Yoga Teacher (RYT 200). Her goal is to help people become healthier both physically and mentally, instead of encouraging them to pursue a certain body image. Along with her internship at BALANCE, Enchi works as a Research Assistant and Crisis Counselor to prepare herself for the future career as a Clinical/Counseling Psychologist.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Bulimia nervosa—Diagnosis and treatment—Mayo Clinic. (n.d.). Retrieved July 1, 2020, from https://www.mayoclinic.org/diseases-conditions/bulimia/diagnosis-treatment/drc-20353621
Crow, S. J., Peterson, C. B., Swanson, S. A., Raymond, N. C., Specker, S., Eckert, E. D., &
Huas, C., Godart, N., Caille, A., Pham‐Scottez, A., Foulon, C., Divac, S. M., Lavoisy, G., Guelfi,
J.-D., Falissard, B., & Rouillon, F. (2013). Mortality and Its Predictors in Severe Bulimia Nervosa Patients. European Eating Disorders Review, 21(1), 15–19. https://doi.org/10.1002/erv.2178
Mitchell, J. E. (2009). Increased Mortality in Bulimia Nervosa and Other Eating Disorders. American Journal of Psychiatry, 166(12), 1342–1346. https://doi.org/10.1176/appi.ajp.2009.09020247